Ticks
In Canada, climate change has contributed to an increased number of ticks, and consequently, tick-borne diseases. Ticks are small arachnids that can sense body heat and must climb onto their host, as they are unable to fly.
Although ticks can attach to any part of the body, they often crawl to warmer areas (e.g., groin, armpit, scalp), making them difficult to spot. Ticks use their mouths to cut the skin and feed on the blood of the host for several days until fully engorged, at which point they drop off.

Tick bites do not cause pain to the host at the time of attachment, but may cause a hypersensitivity reaction, including minor swelling, itching or inflammation, at the site within 24 hours of the bite. This reaction is <5 cm in diameter, does not expand over time and subsides within 1–2 days. The larger danger with ticks is that they can carry infections. Lyme disease is the most common tick-borne disease in Canada. Treatment of Lyme disease involves use of antibiotics (doxycyline, amoxicillin, cefuroxime axetil, ceftriaxone).
Prevention:
- Avoid walking through grassy areas, remain in the middle of pathways.
- Clear away leaf debris.
- Ensure pants and shirts are tight at the ankles and wrists or tucked into socks or gloves.
- Wear light-coloured clothes to see ticks more easily.
- Inspect clothing before returning indoors; once inside, remove clothing and check the whole body, especially tick-prone areas such as ankle, wrist and neck and then shower within 2 hours.
- Inspect pets before returning indoors.
Preventing tick-borne diseases if bitten:
- Remove any attached ticks as soon as they are discovered. Use tweezers and pull straight up (no twisting or angles) to ensure removal of the mouth parts that are embedded in the skin; dispose of tick safely.
- Prompt removal will lessen the severity of any local reaction to a tick bite and reduce the chances of disease transmission.
Mosquitos
Female mosquitos insert the tip of their mouths into small blood vessels near the surface of the skin. Then they inject salivary secretions that commonly cause local histamine reactions (inflammation, swelling, intense itchiness).
Itchy bumps develop within minutes of a bite and may appear as red spots on lighter skin or dark spots or like a bruise on darker skin. They subside slowly over a few days. Some people may develop antibodies that contribute to formation of large welts that last for several days, but anaphylaxis is rare. For most people, the worst they can expect from a mosquito bite is an infection due to scratching at the bite.

However, in different climates, a number of viral and parasitic diseases can be carried by infected mosquitoes (e.g., malaria, Zika virus, Dengue). In Canada, the most relevant mosquito-borne illness West Nile virus. Symptoms usually appear within 2–15 days of being infected. Mild cases may present with fever, body aches, headache, rash, or swollen lymph glands.
Symptoms of more severe illness can include the sudden onset of headache, high fever, stiff neck, vomiting, confusion, vision loss and muscle weakness. Elderly, immunocompromised or chronically ill persons have an increased risk of becoming severely ill after being infected. There is no specific treatment for West Nile virus. Patients with severe symptoms are managed with supportive therapy.
Prevention:
- Eliminate sources of standing water, such as rain barrels, clogged gutters, and bird baths, to prevent breeding.
- Avoid infested areas such as tall grasses, marshes, swamps, bushes, especially at dawn and dusk when mosquitoes are most active.
- Cover the body with a hat, long-sleeved shirt, and long pants; use mesh netting over infants <6 months.
- Use window screens to keep mosquitoes outside.
- Avoid being outside at dawn and dusk.
Bees/Wasps
There are 3 families of insects known to cause a reaction: bees (bumblebees, honeybees), wasps/vespids (including yellow jackets and hornets) and stinging ants (fire ants). Honeybees and bumblebees rarely sting unless they are provoked or feel the need to protect their nests. Honeybees are able to sting only once, as their stinger is barbed and remains embedded in the skin, whereas wasps are able to sting multiple times.

The venom of bees and wasps contains multiple protein allergens, which lead to a severe reaction in those who are susceptible. The most common reaction to a sting is a local reaction (pain, inflammation and swelling at the site of the sting) beginning within minutes of the sting and resolving within a few hours.
Occasionally, there may be a large local reaction that includes swelling over a large area (>10 cm in diameter) with itching and pain that peaks at 24–48 hours after the bite and subsides over 3–10 days. The most serious reaction to bee or wasp stings is anaphylaxis, which can occur within minutes or up to several hours after the initial sting.
Prevention:
- Avoid the use of scented products, as they may attract bees and wasps.
- Avoid eating outdoors or use caution; ensure drinks are covered to avoid swallowing bees and wasps.
- Limit time outdoors at dawn and dusk when bees and wasps are most active.
- Wear clothing that covers as much skin as possible; use mesh netting/screen over children’s cribs, playpens, and strollers.
- Use window screens to keep bees and wasps outside.
- Do not swat at bees or wasps, as it provokes or threatens them; if found in a vehicle, gently guide to an open window.
Spiders

The most common types of spiders in Canada (e.g., wolf, cellar, house, fishing) rarely bite humans unless they feel threatened. Their venom causes only mild redness or swelling. They do not cause disease and are not considered a threat to humans. Spiders in the black widow family (Latrodectus species) can be found in the southernmost parts of British Columbia east to Ontario. Black widow species tend to live in dark places (crawl spaces, woodpiles, basements) and usually bite only to protect themselves or their nests.
The bite feels like a sharp sting that becomes numb initially followed by becoming painful at the bite site. Within 30–60 minutes, the skin may become inflamed and appear red in lightly pigmented skin or have a purple, brown or grey hue in darkly pigmented skin. Severe symptoms can arise within 1–6 hours and may include sweating, nausea, restlessness, muscle spasms, and pain in the lower back or stomach.
Treatment is symptomatic and includes washing the bite area, applying ice to any swelling and managing pain.
Prevention:
- Wear gloves, long-sleeved shirts and long pants tucked into socks when working in areas where spiders are commonly found.
- Keep areas where spiders might be clear of debris (e.g., crawl spaces, wood piles, basements)
- Inspect and shake out gloves, clothing, blankets, and rags prior to use.
Seal doors, windows, and crawl spaces to reduce the chances of a recluse spider entering the home.
Patient Assessment
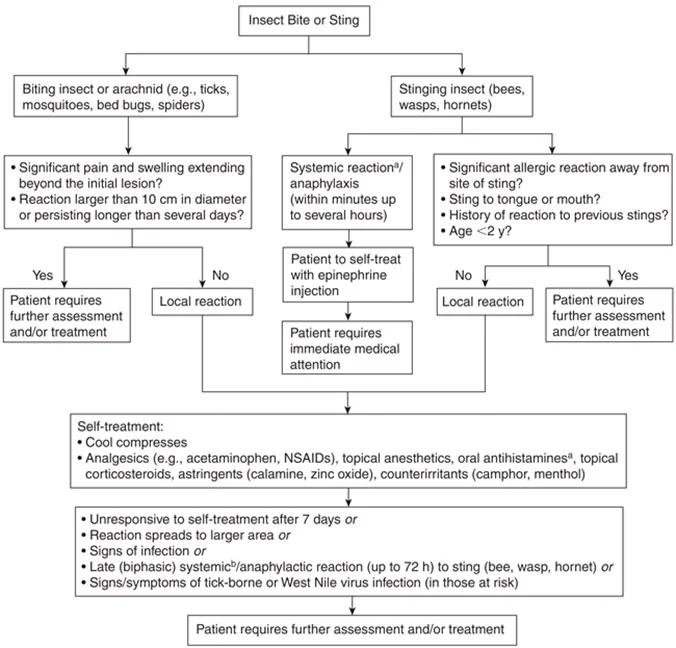
Self-management is appropriate for most arachnid and insect bites or stings because self-limiting localized skin reactions (itching, inflammation, and swelling at the bite site) are the most common consequence. Mild allergic reactions (hives, rash, and mild swelling at the bite site) can also be self-treated. Medical treatment is required if large local reactions (swelling beyond the bite site), multiple stings or an anaphylactic reaction (difficulty breathing, swelling of throat, large areas of swelling or fainting) is experienced.
Insect Repellants
Insect repellents are chemicals used to discourage insects and arachnids from landing or climbing onto the surface on which the repellent has been applied. Insect repellents can be chemicals intended for application to the skin or clothing (DEET, icaridin, oil of lemon eucalyptus, oil of citronella, soybean oil), or insecticides intended for application only to clothing, hats, or other surfaces, not directly to the skin (metofluthrin, permethrin).
Pharmacologic Treatment
Self-treatment of arachnid and insect bites and stings includes relief of pain, swelling and itching using the pharmacologic choices described below.
- Oral analgesics, acetaminophen or NSAIDs can be helpful for associated pain.
- Non-sedating oral antihistamines (e.g., loratadine, cetirizine) are effective for relieving mild to moderate itching. First-generation antihistamines (e.g., diphenhydramine, chlorpheniramine) are also effective but cause more sedation and have a shorter duration of action.
- Topical diphenhydramine is not recommended, as it can cause allergic contact dermatitis and sensitization.
- Topical local anesthetics (e.g., benzocaine, lidocaine, pramoxine), astringents (e.g., calamine, zinc oxide), counterirritants (e.g., camphor, menthol) or ammonia/baking soda combinations (e.g., Afterbite) may provide temporary relief, but evidence of effectiveness or comparative efficacy among these products is lacking.
- Topical corticosteroids can be used for 5–7 days to relieve itch, swelling and irritation in mild to moderate local reactions.
- Oral prednisone (0.5–1 mg/kg up to a maximum of 60 mg) for 3 to 5 days may be required for large local reactions after assessment by an appropriate health-care provider.
Ensure tetanus immunizations are up to date. Arachnid and insect bites, particularly those where a significant lesion develops or necrotic tissue is present (e.g., brown recluse spider), are considered a risk factor for tetanus.